A Patient's Guide to Spondyloarthropathies

Introduction
There are many different types of rheumatological diseases that affect the spine. A rheumatological disease is a problem that affects the entire body as a whole - such as the relatively well known rheumatoid arthritis. When a rheumatological disease affects the spine, the resulting conditon is called a spondyloarthropathy. The term is made up of Greek words: "Spondylo" means "vertebra," "arthro" means "joint" and "pathos" means "disease."
The most common diseases in the spondyloarthropathies include:
- Ankylosing Spondylitis (AS)
- Psoriatic Arthritis (PsA)
- Reactive Arthritis (ReA)
- Enteropathic Arthritis (EA)
- Rheumatoid Arthritis (RA)
This guide will help you understand
- which parts of the spine are affected
- what causes these diseases
- what the most common symptoms are
- what tests your doctor may recommend
- what treatment options are available
Anatomy
What parts of the spine are involved?
This group of diseases cause damage by creating inflammation that attacks the connective tissues of the body. In most cases, the cause of these diseases is unknown. There is increasing evidence that the underlying cause may be a combination of genetics and infection. A person born with certain genes may react differently to certain types of infections. Once that person is exposed to certain infections, the body responds by defending itself. The way the body defends itself against infection is through an inflammatory response. This is normal. What is not normal is that long after the infection
is gone, the inflammation continues. This chronic inflammation causes damage to many of the connective tissue structures in the body and leads to the symptoms.
There are several rheumatological diseases that can affect the spine. The rheumatological diseases that affect the spine primarily affect the connective tissues. One of the most common rheumatological diseases is rheumatoid arthritis (RA). RA primarily attacks the synovial joints.
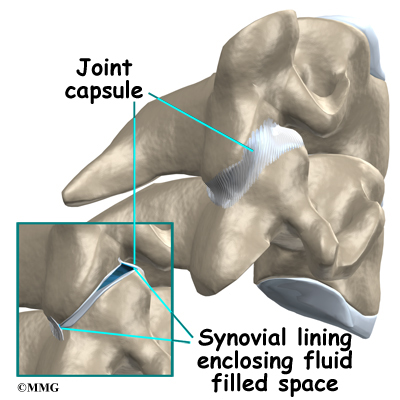
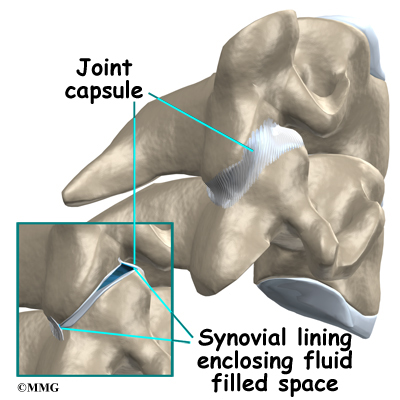
Most of the joints in the body are synovial joints - such as the knee, hip and shoulder. A synovial joint is where two bones come together to form a connection that needs to be flexible - the two bones need to move against one another. The ends of the bones are covered with articular cartilage. Articular cartilage is a white, shiny material that is very slippery. It provides shock absorption and allows the bones to glide against one another easily. The synovial joint is completely enclosed by a joint capsule made up of tough connective tissue on the outside and a thin layer of tissue on the inside called the synovial lining. The joint is water tight. Inside the joint there is a small amount of fluid called synovial fluid. Articular cartilage does not have any blood vessels. The synovial fluid brings nutrients to the articular cartilage as it lubricates the joint.
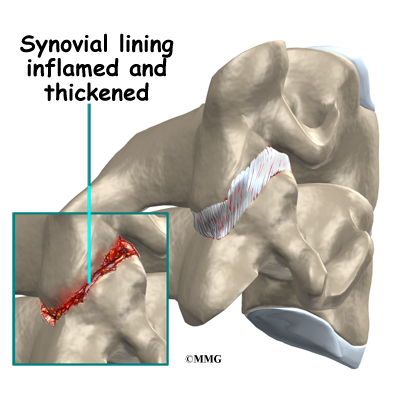
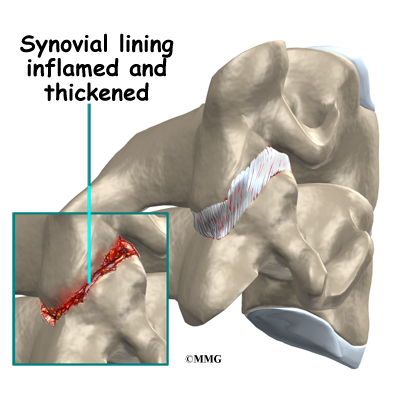
In RA, the synovial lining of the joint is affected. The normally thin tissue of the synovial lining becomes inflamed and thickened. This material begins to produce inflammatory chemicals that damage the articular cartilage and bone underneath. The joint is slowly destroyed until bone rubs against bone. There are synovial joints between each vertebra in the spine and between the skull and the first cervical vertebra. It is easy to see why RA affects the spine.
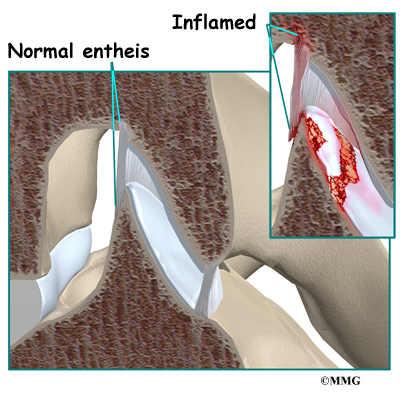
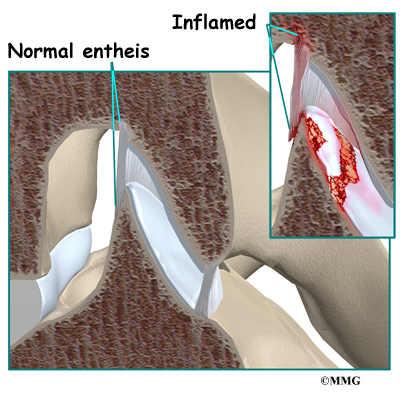
In some rheumatological diseases, the inflammatory process affects other connective tissue structures. One structure that is commonly affected is where ligaments and tendons attach to the bone. This area is called an enthesis. There are entheses located all over the body - wherever tendons and ligaments need to attach to bone. There are also many entheses in the spine itself, such as where the intervertebral disc attaches to the vertebra. Many of the rheumatological diseases that affect the spine seem to attack these areas of the spine. It is unclear why this occurs.
Related Document: A Patient's Guide to Lumbar Spine Anatomy
Causes
What causes this problem?
The cause, or causes, of all of these rheumatological diseases is still unknown. There is increasing evidence that the underlying cause in many of these conditions is a combination of a person's genetic makeup and how that person responds to certain types of infections.
For many years, doctors have been aware that people with these diseases have a higher percentage of a gene called HLA-B27. The HLA-B27 gene plays a role in determining how the cells of the body react against infection. Not everyone with this gene will develop a rheumatological disease, but the vast majority of people with any of the diseases have the gene. Recently, more research has shown that there are a number of variations of the HLA-B27 gene. This further complicates a very complex situation in trying to understand what role genetics plays in the cause of these diseases.
There are also a number of different infections that have been found to be related to the development of the rheumatological diseases. When patients with these diseases are studied, there seems to be certain bacterial infections that are more likely to precede the development of the rheumatological disease. The infection may be over, but the body continues to mount an inflammatory response that instead attacks the connective tissue
structures of the body itself.
The current evidence suggests that people with certain genes are more likely to react to certain types of infections by developing a rheumatological disease.
Related Document: A Patient's Guide to Rheumatoid Arthritis
Symptoms
What does the condition feel like?
Most of these diseases cause pain and stiffness as the primary symptoms affecting the spine. The pain and stiffness is worse in the morning and improves with activity. The flexibility of the spine decreases as time passes and the disease progresses.
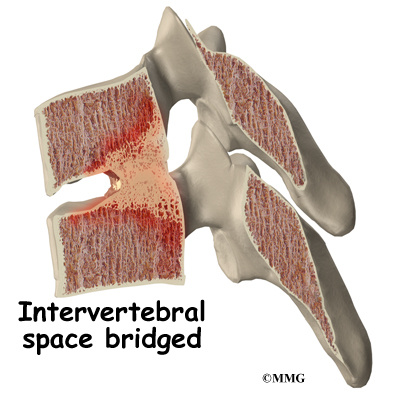
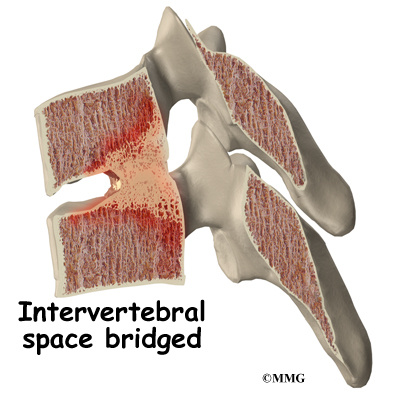
In diseases that affect the synovial joints, destruction of the joints can result in instability of the spine and may cause pressure on the spinal nerves or spinal cord. In the
diseases that affect the entheses, the spine more commonly develops large bone spurs and may fuse together and become stiff. Instability occurs if the stiff spine is fractured.
Because these diseases are systemic, meaning that they affect the entire body, the symptoms also affect the entire body. The symptoms include pain in areas that are affected, such as the other synovial joints, and the other entheses of the body.
Besides back pain, sacroiliac, hip, and shoulder pain are also common. The exact location of symptoms depends on the type of spondyloarthropathy (SpA) present. Some of the diseases may include a skin rash, such as psoriasis. Several of the spondyloarthropathies affect the eyes, causing uveitis (inflammation of the iris). Inflammation of the urethra (the tube from the bladder to the outside) can cause pain when urinating, called urethritis. Ankylosing Spondylitis (AS) can also affect the gut, aorta, or heart. All of the symptoms mentioned here are called extraskeletal manifestations. This means the symptoms affect some part of the body other than the tendons and bones.
Diagnosis
How do doctors diagnose the problem?
The diagnosis requires a careful history followed by a thorough physical examination. Many patients have someone directly related to them that suffers from the same disease. Your doctor may ask questions about symptoms of recent infections such as diarrhea, burning with urination, difficulty with vision and eye pain.
The laboratory evaluation is very useful in the diagnosis. Tests such as C-reactive protein (CRP) level and erythrocyte sedimentation rate (ESR) may be ordered to look for signs of infection and chronic inflammation other tests can be done for rheumatoid arthritis and the presence of the HLA-B27 gene. The HLA-B27 gene is not always present in patients with spondyloarthropathy. And it may be present in normal, healthy individuals without spondyloarthropathies.
Analysis of synovial fluid may be needed to rule out septic (infectious) arthritis. Additional tests may be ordered for patients with inflammatory bowel disease (IBD) or when reactive arthritis is suspected.

X-rays can be very useful to show the changes in the spine, joints and pelvis that are common with many of these diseases. X-rays are usually the first test ordered before any of the more specialized tests. In the early stages the x-rays may be negative, but as time passes, the changes may appear and confirm the diagnosis.
Other radiological imaging tests may be useful. A bone scan can show the sites of inflammation before the changes appear on x-rays. A bone scan is a special test where radioactive tracers are injected into your blood stream. The tracers then show up on special x-rays of your back. The tracers build up in areas where bone is undergoing a rapid repair process, such as a healing fracture or the area surrounding an infection or tumor. Usually the bone scan is used to locate the problem. Other tests such as the computed tomography (CT) scan or magnetic resonance imaging (MRI) scan are then used to look at the area in detail.
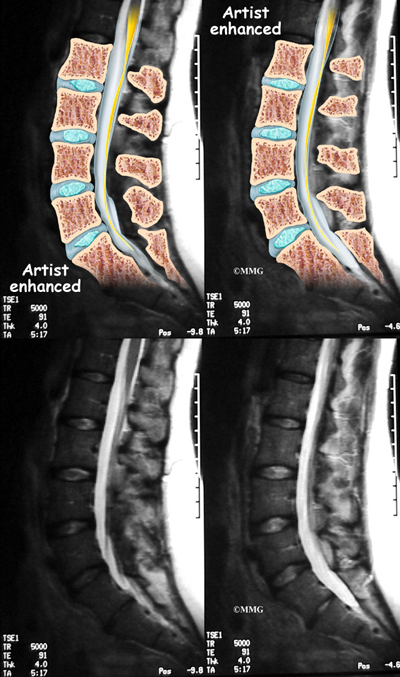
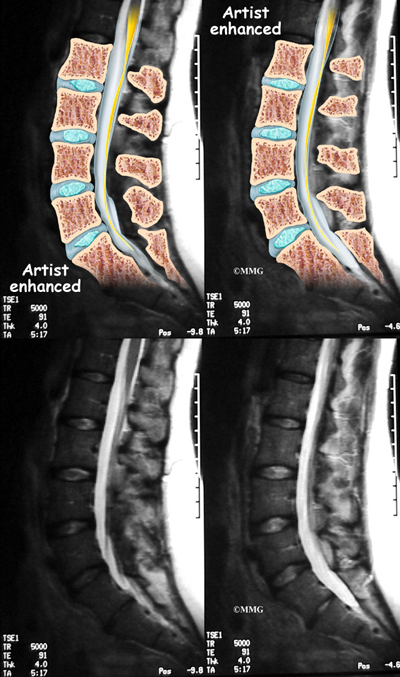
If there are symptoms suggesting the spinal nerves or spinal cord are in danger, an MRI scan may be recommended to look at the spine more closely. The MRI scan uses magnetic waves to create pictures of the lumbar spine in slices. The MRI scan shows the lumbar spine bones as well as the soft tissue structures such as the discs, joints and nerves. MRI scans are painless and don't require needles or dye. Specialized MRI techniques are now available that can detect inflammatory changes in the sacroiliac and vertebral joints long before they appear on x-rays.
Treatment
What treatment options are available?
There is no cure for any of these diseases. The goal of treatment is to manage the pain and, when possible, to slow the progression of the damage to the underlying structures.
Remaining as active as possible is critical to maintaining your function. A physical therapy program can teach you how to maximize your function and retain as much flexibility as possible. Learn all you can about what you can do to control your symptoms and remain as healthy as possible.
If you smoke or use tobacco products, long-term outcomes are worse. You should quit as soon as possible. Your doctor can help you with this important step.
Medications are the primary tools available for treatment. Non-steroidal anti-inflammatory drugs (NSAIDs) are the main drugs used for treatment of the pain associated with these diseases. These drugs include aspirin, ibuprofen, indomethacin and naprosyn. There are others in the group as well. These drugs reduce the inflammation and control pain. There is no evidence that they stop or slow the progression of the disease.
Cortisone can be used to control flare-ups of pain. Cortisone is a powerful anti-inflammatory medication. When used for short periods of time, the medication is safe and well tolerated. When used continuously over a period of months, the side effects can be significant. Your doctor will probably not want to use cortisone if possible. In some cases, such as with advanced rheumatoid arthritis it may become necessary to use cortisone indefinitely to control the disease.
There are newer medications that have been developed to control rheumatoid arthritis that are sometimes beneficial in the spondyloarthropathies. Some of these medications actually slow the progression of the damage from the disease. These medications are known as disease modifying anti-rheumatic drugs (DMARDs). DMARDs include gold injections, methotrexate, sulfasalazine and azothioprine. These medications may be used primarily to control the symptoms in other parts of the body, but may also improve the spinal disease as well.
Recently, new medications have been available that may prove to be very beneficial for these diseases. One of the chemicals that seems to make the inflammation worse in these diseases is tumor necrosis factor (TNF). Drugs that block the effect of this chemical are called tumor necrosis factor-a inhibitors. TNF-a inhibitors are used to treat a variety of inflammatory diseases. These have recently begun to be used to treat a variety of inflammatory diseases. These drugs have shown promise in helping control the inflammation and symptoms of the spondyloarthropathies as well. TNF-a inhibitors result in dramatic decreases in CRP levels and ESR improvements are also seen on MRIs.
Treatment with TNF-a inhibitors must be kept up over the long-term to stay in control of the disease. If one agent doesn't work, your doctor may switch you to another. There are some serious side effects with these agents, so they aren't used with everyone. We don't know yet if these agents will prevent the bony changes that lead to spinal fusion. More study is needed to determine this.
Surgery is rarely indicated in the treatment of these diseases, except where the damage caused by the disease has caused pressure on the spinal nerves or spinal cord. Total joint replacement may be needed for patients with severe damage to the hip or knee. Some patients elect to have surgery to correct kyphosis (forward curve or humpback of the upper spine) or to correct spine instability from fracture.
Finally, learning as much as you can about how you can take care of yourself is an important part of managing these chronic diseases. Support groups are available online and in many cities where people can come together and help with information and support. There is nothing as valuable as getting advice and guidance from someone who has experience with the disease and can provide tips and pointers for living with the disease on a daily basis. It is always nice to know that you are not alone.
|