A Patient's Guide to Septic Arthritis
Introduction
Septic arthritis is an infection inside a joint that is caused by bacteria. (Septic describes an infection in the body caused by bacteria.) It comes on suddenly and causes very noticeable pain and swelling in the affected joint. It can affect anyone, including infants and children. But it is most likely to affect people over 60 and people with certain health or joint problems.
This guide will help you understand
- how septic arthritis develops
- how doctors diagnose the condition
- what can be done for septic arthritis
Anatomy
Where does septic arthritis develop?
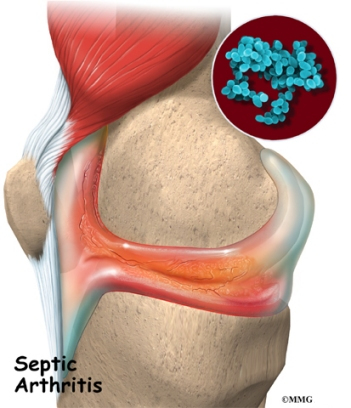
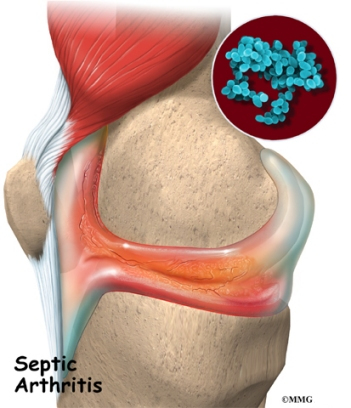
In septic arthritis, the synovial fluid--the lubricating fluid inside a joint--becomes contaminated, or infected, with bacteria. In response to the infection, the body produces white blood cells that try to fight and kill the bacteria. This creates pus that mixes with the synovial fluid inside the joint. The white blood cells that fight infection produce chemicals that may not only kill the bacteria but may also damage the joint surfaces. Once this process begins, the breakdown of the joint can continue even after the infection goes away and the bacteria are all dead.
About 80 percent of cases of septic arthritis involve only one joint. Roughly half of the time a knee is affected. The other most common sites are the hip, shoulder, wrist, ankle, elbow, and small joints in the hands and feet. When more than one joint is affected, the knees are usually involved.
Causes
Why do I have this problem?
The cause of septic arthritis is known. It is caused by a bacterial infection in a joint. Bacteria can get into a joint in many ways. The bacteria may be introduced into the joint as a result of injury, such as a laceration that goes into the joint. Surgery on the joint can introduce bacteria into the joint. There is always a small chance of causing an infection if a needle is placed in the joint to either remove synovial fluid for testing or to inject medications into the joint. The joint infection can also come from infections in the skin around the joint or infections in the bones around the joint. The bacteria can also be carried by the blood from an area of infection somewhere else in the body. Once in the joint, synovial fluid provides a good place for the infection to lodge and grow.
Although they do not cause septic arthritis, several risk factors make it more likely to develop. These risk factors include a suppressed immune system, drug abuse, and other diseases. Other diseases that go along with septic arthritis include rheumatoid arthritis, diabetes, cancer, sickle cell disease, anemia, lupus, liver disease, skin infections, and hemophilia.
Artificial joints and recent joint surgery or arthrocentesis (inserting needles into the joint) are also risk factors for septic arthritis. However, the risk from these sources is small. The rate of septic arthritis from artificial joints is less than one percent. The rate following corticosteroid injections is less than 0.01 percent. Rates of septic arthritis following arthroscopy (surgery conducted using a small TV camera inserted into a joint) range from 0.04 percent to four percent. Septic arthritis caused by arthroscopy usually begins within two weeks of the procedure.
The biggest risk factor in septic arthritis is advanced age. Roughly half the cases of septic arthritis occur in people over age 60. In these patients, 75 percent of the infections occur in joints that have already been affected by arthritis, especially the hips, knees, and shoulders.
Symptoms
What does septic arthritis feel like?
Septic arthritis causes moderate to severe joint pain that comes on from a few hours to a few days. (Doctors refer to this as acute onset.) The pain is much worse when you move or touch the joint. The joint is usually warm and red, and it can't move easily. You may have other evidence of infection, including a fever, chills, flu-like symptoms, and high white blood cell counts. However, 20 percent of patients with septic arthritis run no fever. Even fewer people over 60 run a fever or have high white blood cell counts when they have septic arthritis.
Diagnosis
How do doctors identify the condition?
The sooner a diagnosis of septic arthritis is made, the better. The more time the infection goes unchecked, the more damage it can do to the joint.
If you have acute onset in one joint and a risk factor of any kind, your doctor will probably test for septic arthritis. A needle will be inserted into the joint and synovial fluid removed and sent to the lab. Your doctor will perform several tests on the synovial fluid. The most important test is probably the measuring the white blood cell count in the fluid. An infection in the joint causes the white blood cell count to be extremely high. Other tests are also useful especially making sure there are no crystals in the fluid that could indicate the presence of gout. A gout attack can easily be mistaken for an infection, and vice versa.
The fluid will be examined under a microscope to look for bacteria. Your doctor will also have the lab perform a culture of the synovial fluid to try and grow the bacteria. In this test a small sample of the fluid is placed in a special container and allowed to incubate in a warm cabinet. The test usually takes from 24 to 36 hours to see if any bacteria grow. This test can also help determine the specific type of bacteria that is causing the infection. If bacteria grow in culture the lab can also test different antibiotics on the bacteria to see which antibiotic will work the best.
Your doctor may ask you to have an X-ray. The X-ray will be used to look for any problems in the joint. It will also provide a baseline of information so your doctor can see the changes in your joint over the course of the infection.
Treatment
What can be done for septic arthritis?
Your doctor will prescribe an antibiotic right away, taking into account your medical history, other diseases or infections you have, and the lab test results. The antibiotic may be changed as your doctor gets information from the testing of the synovial fluid. You will probably be started on intravenous (IV) antibiotics. You will need to continue on oral antibiotics for up to six weeks.
Antibiotics alone may not get rid of septic arthritis. The fluid in the joint may need to be drained at least once a day to remove the pus. This can be done using a large needle. In larger joints such as the knee, arthroscopy may also be used to wash the joint out and remove dead or damaged tissue. Surgery may be necessary to drain and clean joints such as the hip and shoulder. Surgery may also be necessary in joints with bone infections and in joints where the infection can't be easily controlled.
As your infection begins to clear up, your doctor may suggest that you begin strengthening and range of motion exercises. They will help your joint regain its strength and flexibility. A physical or occupational therapist may oversee your exercise program.
How well your septic arthritis responds to treatment will depend on a number of factors. Most important is how soon you got treatment. Only about 25 percent of patients who wait a week to see a doctor can hope for a complete recovery. So you may feel as though your doctor is rushing you through tests and treatment, but it is for a very good reason.
|