A Patient's Guide to Pain Management: Facet Joint Injections
Introduction
Injections are commonly used by pain specialists, both to help diagnose the painful condition and to help treat the painful condition.
Facet joint injections are commonly used to determine what is causing back pain. Facet joint injections are primarily diagnostic injections, meaning that they help your doctor determine the cause of your back pain but may not provide you with any long-term relief from the pain. These injections eliminate pain temporarily by filling the facet joint with an anesthetic medication that numbs the facet joint, the ligaments, and joint capsule around the facet joint. If the facet joint is injected and your pain goes away for several hours, then it is very likely that the joint is causing your pain. Once you and your doctor know what structure is causing your pain, you can begin to explore options for treating the condition.
This guide will help you understand:
- where the injection is given
- what your doctor hopes to achieve
- what you need to do to prepare
- what you can expect from the injection
- what might go wrong
Anatomy
What parts of the body are involved?
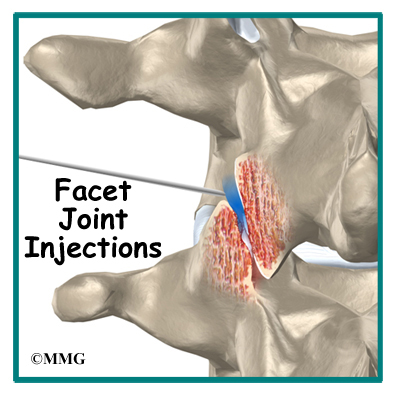
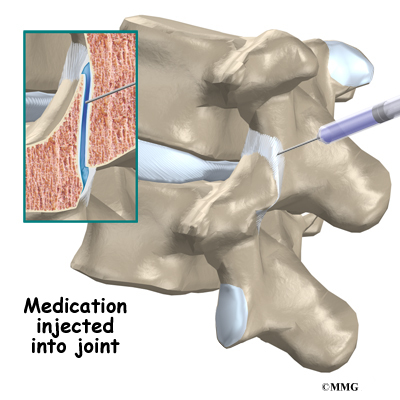
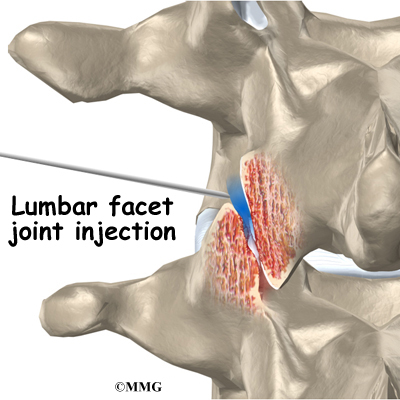
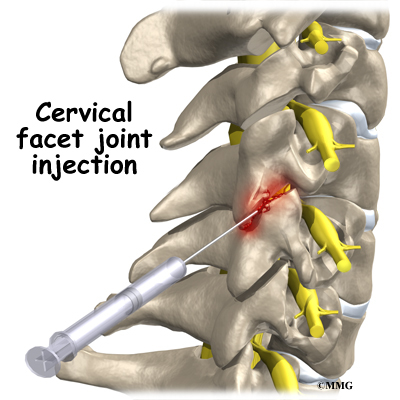
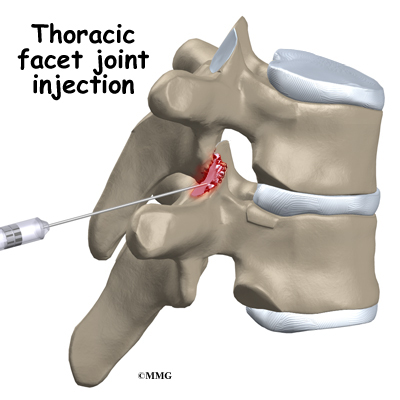
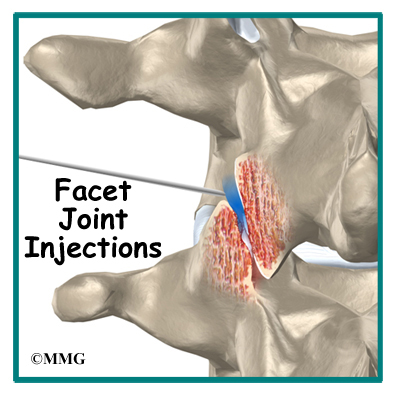
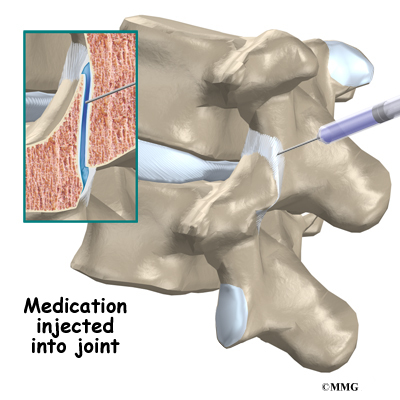
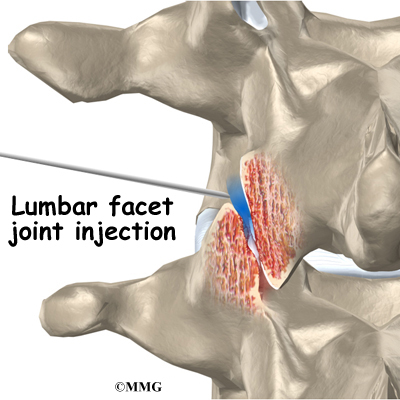
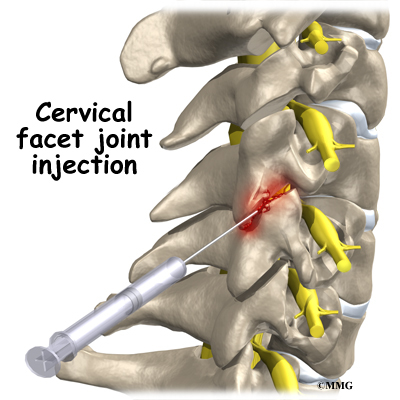
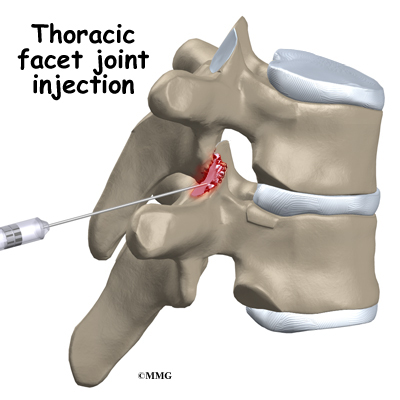
To perform a facet joint injection, your doctor inserts a needle into the facet joint so that the tip of the needle is inside the joint.
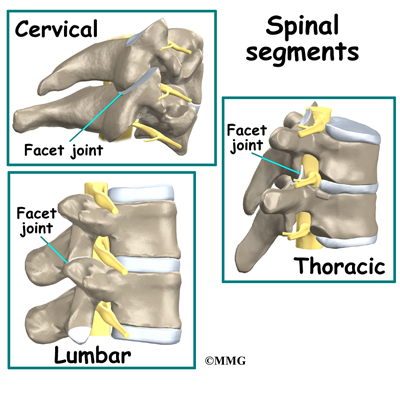
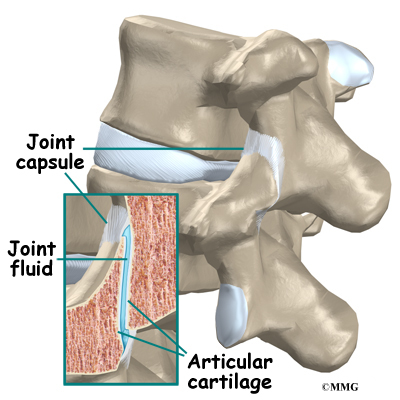
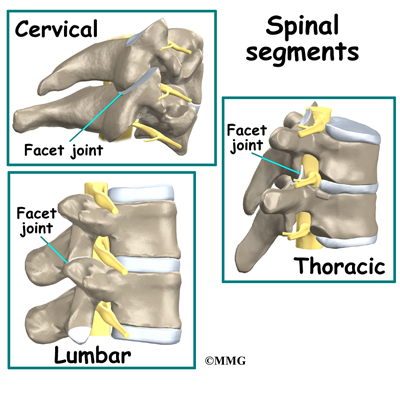
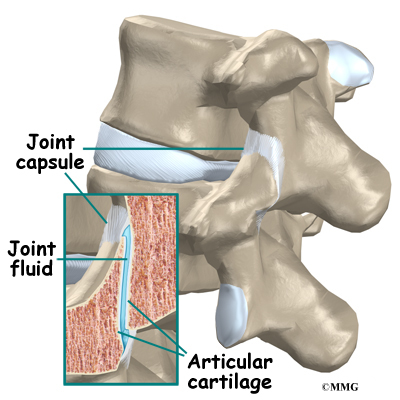
A facet joint is a small, bony knob that extends out from the vertebral body. Where these knobs meet, they form a joint that connects the two vertebrae. The surface of the facet joints are covered by articular cartilage. Articular cartilage is a smooth, rubbery material that covers the surface of all synovial joints. It allows the bone ends to move against each other smoothly without friction.
Each joint is surrounded by a joint capsule. The joint capsule is made up of the ligaments and connective tissues that help hold the joint together. The joint capsule forms a water tight sac that contains the joint fluid. The facet joints allow freedom of movement as you bend forward and back.
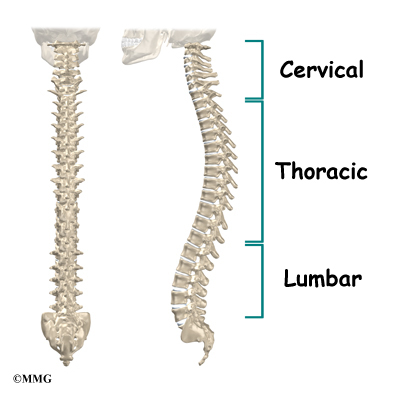
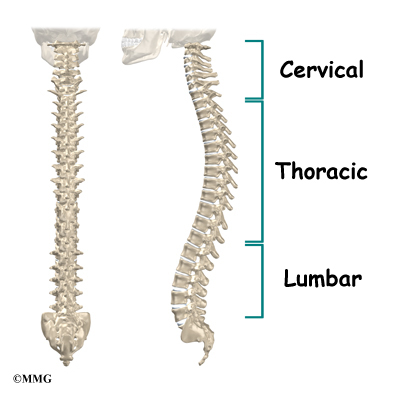
There are two facet joints between each vertebrae of the spine. The facet joints are located on the back of the spinal column in the lumbar and thoracic spine. In the neck, or cervical spine, they are located on the each side of the vertebra.
Like all joints, the facet joint can wear out - or degenerate. This condition is sometimes called degenerative arthritis or osteoarthritis. When this occurs in the facet joints it can cause back pain. In addition to back pain, the pain may radiate into the buttock and back of the thigh.
Related Document: A Patient's Guide to Lumbar Spine Anatomy
Rationale
What does my physician hope to achieve?
Your doctor is recommending a facet joint injection to try and determine if the joints are the cause of your back pain. This type of injection is primarily a diagnostic injection. The injection may only reduce your pain temporarily, maybe only for a few hours. Once your doctor is sure that it is the facet joint causing your pain, other procedures may be recommended to reduce your pain for a longer period of time.
During a facet joint injection, the medications that are normally injected include a local anesthetic and cortisone. The anesthetic medication, such as lidocaine or bupivicaine, is the same medication used to numb an area when you are having dental work or having a laceration sutured. The medication causes temporary numbness lasting one hour to six hours, depending on which type of anesthetic is used.
Cortisone is an extremely powerful anti-inflammatory medication. When this medication is injected into a painful, inflamed joint, it can reduce the inflammation and swelling. Reducing the inflammation reduces pain. If cortisone is also injected into the joint at the same time, you may get several weeks of relief from your pain. This can allow you to get started in a physical therapy program, strengthen the muscles, and begin normal movement again. When the cortisone wears off, the pain may not return.
Related Document: A Patient's Guide to Facet Joint Arthritis
Preparations
How will I prepare for the procedure?
To prepare for the procedure your doctor may tell you to remain "NPO" for a certain amount of time before the procedure. This means that you should not eat or drink anything for the specified amount of time before your procedure. This means no water, no coffee, no tea - not anything. You may receive special instructions to take your usual medications with a small amount of water. Check with your doctor if you are unsure what to do.
You may be instructed to discontinue certain medications that affect the clotting of your blood several days before the injection. This reduces the risk of excessive bleeding during and after the injection. These medications may include the common Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) such as aspirin, ibuprofen, naproxen, and many other medications that are commonly used to treat arthritis. If you are taking any type of blood thinning medication you should let your doctor know. You will most likely need to have this medication regulated or temporarily discontinued prior to the injection. Your doctor will need to determine if it is safe to discontinue these medications in order to have the injection.
You may need to arrange to have transportation both to and from the location where you will undergo the injection. Wear loose fitting clothing that is easy to take off and put on. You may wish to take a shower the morning of the procedure, using a bactericidal soap to reduce chances of infection. Do not wear jewelry or any type of scented oils or lotions.
Procedure
What happens during the procedure?
When you are ready to have the injection, you will be taken into the procedure area and an IV will be started. The IV allows the nurse or doctor to give you any medications that may be needed during the procedure. The IV is for your safety because it allows very rapid response if you have a problem during the procedure, such as an allergic reaction to any of the medications injected. If you are in pain or anxious, you may also be given medications through the IV for sedation during the procedure.
Most injection procedures today are done with the help of fluoroscopic guidance. The fluoroscope is an x-ray machine that allows the doctor to actually see an x-ray image while doing the procedure. This allows the doctor to watch where the needle goes as it is inserted. This makes the injection much safer and much more accurate. Once the needle is in the right location, a small amount of radiographic dye is injected. This liquid dye shows up on the x-ray image and the doctor can watch where it goes. The medication used for the injection will go in the same place, so the doctor wants to make sure that the medication will go to the right place to do the most good. Once the correct position is confirmed, the medication is injected and the needle is removed.
You will then be taken out of the procedure room to the recovery area. You will remain in the recovery area until the nurse is sure that you are stable and do not have any allergic reaction to the medications. The anesthetic may cause some temporary numbness and weakness. You will be free to go when these symptoms have resolved.
Complications
What might go wrong?
There are several complications that may occur during or after the facet joint injection. Injection procedures are safe and unlikely to result in a complication, but no procedure is 100% foolproof. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Complications are uncommon, but you should know what to watch for if they occur.
Allergic Reaction
Like most procedures where medications are injected, there is always a risk of allergic reaction. The medications that are commonly injected include lidocaine, bupivicaine, radiographic dye, and cortisone. Allergic reactions can be as simple as developing hives or a rash. They can also be life threatening and restrict breathing. Most allergic reactions will happen immediately while you are in the procedure room so that help is available immediately. Most reactions are treated and cause no permanent harm. You should alert your doctor if you have known allergies to any of these medications.
Infection
Several types of infections are possible complications of facet joint injections. Any time a needle is inserted through the skin, there is a possibility of infection. Before any injection is done, the skin is cleansed with a disinfectant and the health care provider doing the injection uses what is called sterile technique. This means that the needle and the area where the needle is inserted remains untouched by anything that is not sterile. The provider may also use sterile gloves.
Infections can occur just underneath the skin, in a muscle, or in the facet joint. You should watch for signs of increasing redness, swelling, pain, and fever. Almost all infections will need to be treated with antibiotics. If an abscess forms, then a surgical procedure may be necessary to drain the pus in the abscess. Antibiotics will also be necessary to treat the infection.
Nerve Damage
Many pain injections are done close to nerves. The facet joint injection is one of the safest spinal injections because the needle is usually not near the spinal nerves, but the needle used to do the injection may accidentally hit a nerve. This can cause damage to the nerve and result in increased pain. Numbness and weakness may also result. Nerves that have been punctured with a needle will usually recover and do not require any additional surgical procedures.
Increased Pain
Not all injections work as expected. Sometimes, injections cause more pain. This may be due to increased spasm in the muscles around the injection. The increased pain is usually temporary, lasting a few hours or a few days. Once the medication has a chance to work, the injection may actually perform as expected and reduce your pain. Increased pain that begins several days after the injection may be a sign of infection. You should alert your doctor if this occurs.
After Care
What happens after the procedure?
p>You will be able to go home soon after the procedure, probably within one hour. If all went as planned, you probably won't have any restrictions on activity or diet.
Most doctors will arrange a follow-up appointment, or phone consult, within one or two weeks after the injection to see how you are doing and what effect the procedure had on your symptoms. Your doctor will be interested in how much the pain is reduced while the anesthetic (numbing medication) is working. You may be given a pain diary to record what you feel for the next several hours. This is important for making decisions, so keep track of your pain.
One question that always comes up is: How many injections are safe to have? There is no definite answer to that question. Most doctors would recommend that you limit the number of injections to three to five per year. The reason for this limit has to do with how much cortisone is safe to put in your body. Cortisone has bad side effects when you take the medication often, either as a pill or as an injection. These side effects are why doctors do not like to do these injections more often than necessary.
And remember, these injections are not a cure for your pain; they are only a part of your overall pain management plan. You will still need to continue working with the other recommendations from your pain management team.
|