A Patient's Guide to Mallet Finger Injuries
Introduction
When you think about how much we use our hands, it's not hard to understand why injuries to the fingers are common. Most of these injuries heal without significant problems. One such injury is an injury to the distal interphalangeal, or DIP, joint of the finger. This joint is commonly injured during sporting activities such as baseball. If the tip of the finger is struck with the ball, the tendon that attaches to the small bone underneath can be injured. Untreated, this can cause the end of the finger to fail to straighten completely, a condition called mallet finger.
This guide will help you understand
- what parts make up the DIP finger joint
- what types of injuries affect this joint
- how the injury is treated
- what to expect from treatment
Anatomy
What parts of the finger are involved?
The finger joints work like hinges when the fingers bend and straighten. The main knuckle joint is the metacarpophalangeal joint (MCP joint). It is formed by the connection of the metacarpal bone in the palm of the hand with the first finger bone, or proximal phalanx. Each finger has three phalanges, or small bones, separated by two interphalangeal joints (IP joints). The one closest to the MCP joint (knuckle) is called the proximal IP joint (PIP joint). The joint near the end of the finger is called the distal IP joint (DIP joint).
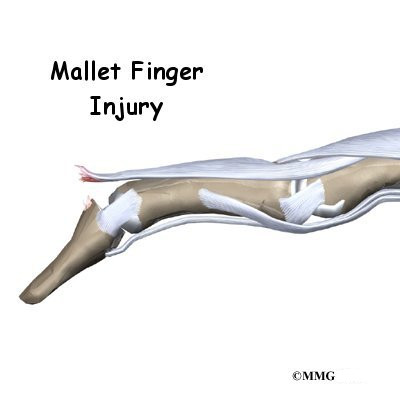
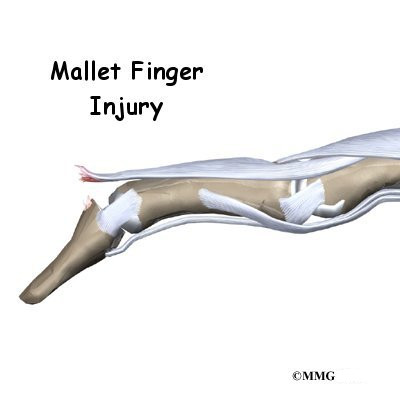
The extensor tendon is attached to the base of the distal phalanx. When it tightens, the DIP joint straightens. Another tendon, the flexor tendon, is attached to the palm of the finger. When it pulls, the DIP joint bends.
Related Document: A Patient's Guide to Hand Anatomy
Causes
How do these injuries of the DIP joint occur?
A mallet finger results when the extensor tendon is cut or torn from the attachment on the bone. Sometimes, a small fragment of bone may be pulled, or avulsed, from the distal phalanx. The result is the same in both cases: the end of the finger droops down and cannot be straightened.
Symptoms
What do mallet finger injuries look and feel like?
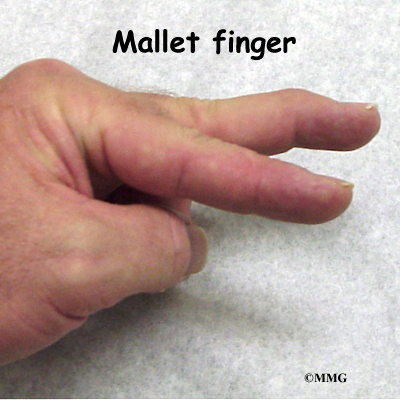
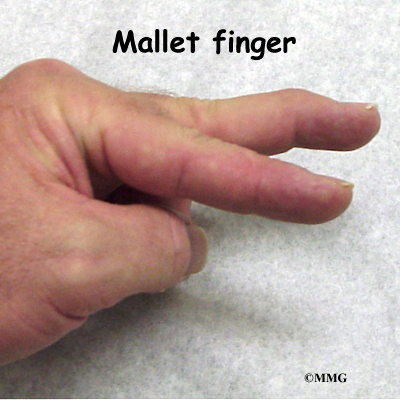
Initially, the finger is painful and swollen around the DIP joint. The end of the finger is bent and cannot be straightened voluntarily. The DIP joint can be straightened easily with help from the other hand. If the DIP joint gets stuck in a bent position and the PIP joint (middle knuckle) extends, the finger may develop a deformity that is shaped like a swan's neck. This is called a swan neck deformity.
Related Document: A Patient's Guide to Swan Neck Deformity of the Finger
Diagnosis
What tests will my doctor do?
Usually the diagnosis is evident from the physical examination. X-rays are required to see if there is an associated avulsion fracture since this may change the recommended treatment. No other tests are normally required.
Treatment
What can be done for the problem?
Nonsurgical Treatment
Treatment for mallet finger is usually nonsurgical. If there is no fracture, then the assumption is that the end of the tendon has been ruptured, allowing the end of the finger to droop. Usually continuous splinting for six weeks followed by six weeks of nighttime splinting will result in satisfactory healing and allow the finger to extend.
The key is continuous splinting for the first six weeks. The splint holds the DIP joint in full extension and allows the ends of the tendon to move as close together as possible. As healing occurs, scar formation repairs the tendon. If the splint is removed and the finger is allowed to bend, the process is disrupted and must start all over again. The splint must remain on at all times, even in the shower.
While a simple homemade splint will work, there are many splints that have been designed to make it easier to wear at all times. In some extreme cases where the patient has to use the hands to continue working (such as a surgeon), a metal pin can be placed inside the bone across the DIP joint to act as an internal splint and allow the patient to continue to use the hand. The pin is removed at six weeks.
Splinting may even work when the injury is quite old. Most doctors will splint the finger for eight to 12 weeks to see if the drooping lessens to a tolerable amount before considering surgery.
Surgery
DIP Fixation
Surgical treatment is reserved for unique cases. The first is when the result of nonsurgical treatment is intolerable. If the finger droops too much, the tip of the finger gets caught as you try to put your hand in a pocket. This can be quite a nuisance. If this occurs, the tendon can be repaired surgically, or the joint can be fixed in place. A surgical pin acts like an internal cast to keep the DIP joint from moving so the tendon can heal. The pin is removed after six to eight weeks.
Fracture Pinning
The other case is when there is a fracture associated with the mallet finger. If the fracture involves enough of the joint, it may need to be repaired. This may require pinning the fracture. If the damage is too severe, it may require fusing the joint in a fixed position.
Finger Joint Fusion
If the damage cannot be repaired using pin fixation, finger joint fusion may be needed. Joint fusion is a procedure that binds the two joint surfaces of the finger together, keeping them from rubbing on one another. Fusing the two joint surfaces together eases pain, makes the joint stable, and prevents additional joint deformity.
Related Document: A Patient's Guide to Finger Fusion Surgery
Rehabilitation
What will my recovery be like?
Nonsurgical Rehabilitation
When the injury is new, the DIP joint is splinted nonstop in full extension for six to eight weeks. A mallet finger that is up to three months old may require splinting in full extension for eight to 12 weeks. The splint is then worn for shorter periods that include nighttime splinting for six more weeks. Skin problems are common with prolonged splinting. Patients should monitor the skin under their splint to avoid skin breakdown. If problems arise, a new or different splint may be needed. Nearby joints may be stiff after keeping the finger splinted for this length of time. Therapy and exercise may be needed to assist in finger range of motion and to reduce joint stiffness.
After Surgery
Rehabilitation after surgery for mallet finger focuses mainly on keeping the other joints mobile and preventing stiffness from disuse. A physical or occupational therapist may be consulted to teach you home exercises and to make sure the other joints do not become stiff. After the surgical pin has been removed, exercises may be instituted gradually to strengthen the finger and increase flexibility.
|