A Patient's Guide to Pain Management: Sacroiliac Joint Injections
Introduction
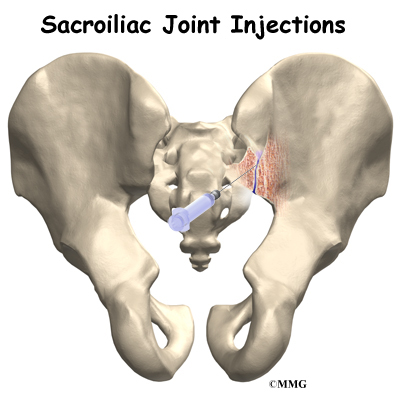
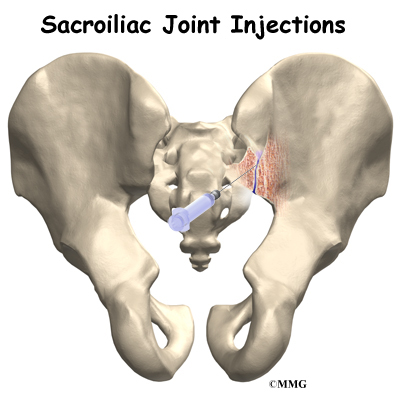
Sacroiliac (SI) joint injections are commonly used to determine what is causing back pain. SI joint injections are primarily diagnostic injections, meaning that they help your doctor determine the cause of your back pain. These injections eliminate pain temporarily by filling the SI joint with an anesthetic medication that numbs the joint, the ligaments, and joint capsule around the SI joint.
This guide will help you understand:
- where the injection is given
- what your doctor hopes to achieve
- what you need to do to prepare
- what you can expect from the injection
- what might go wrong
Anatomy
What parts of the body are involved?
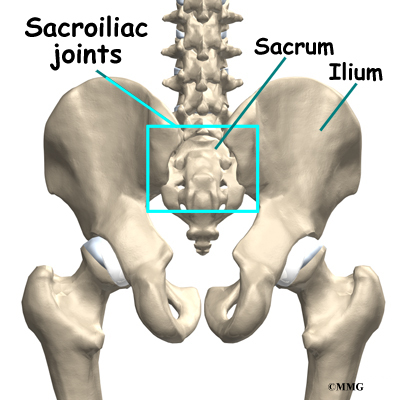
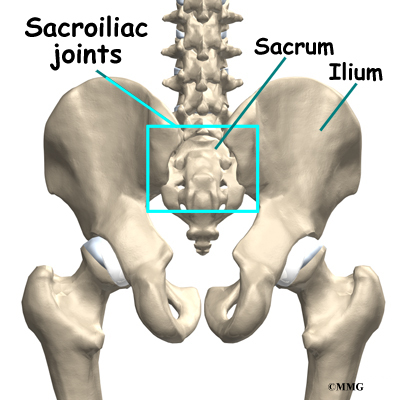
To perform a sacroiliac joint injection, your doctor inserts a needle into the sacroiliac joint. The sacroiliac (also called the SI) joint connects the sacrum and the iliac bone. You can see these joints from the outside as two small dimples on each side of the lower back at the belt line. The sacrum is a triangular-shaped bone formed by the fusion of several vertebrae during development. It sits at the lower end of the spine, just below the lumbar spine.
The SI joint is one of the larger joints in the body. The surface of the joint is wavy and fits together similar to the way two gears fit together. Very little motion occurs in the SI joint. The motion that does occur is a combination of sliding, tilting and rotation. The most the joint moves in sliding is probably only a couple of millimeters, and it may tilt and rotate two or three degrees.
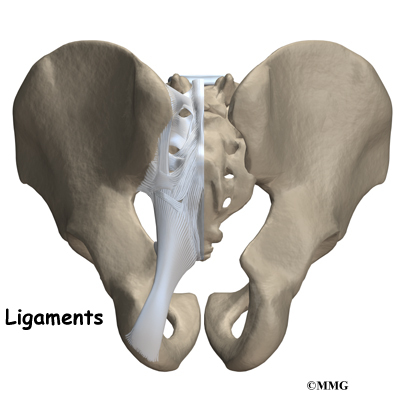
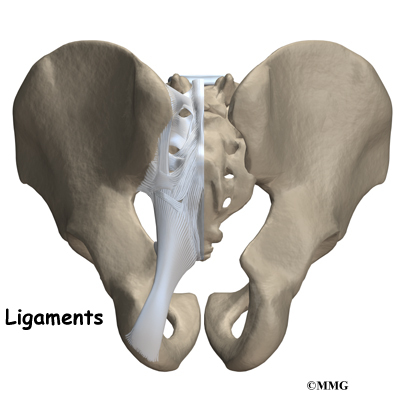
The SI joint is held together by several large, very strong ligaments. The strongest ligaments are in the back of the joint outside of the pelvis. Because the pelvis is a ring, these ligaments work somewhat like the hoops that hold a barrel together. The SI joint hardly moves in adults. It appears that the primary function of the joint is to be a shock absorber and to provide just enough motion and flexibility to lessen the stress on the pelvis and spine.
During the end of pregnancy as delivery nears, the hormones that are produced cause the joint to relax. This allows the pelvis to be more flexible so that birth can occur more easily. Multiple pregnancies seem to increase the amount of arthritis that forms in the joint later in life. Other than the role the joint plays in pregnancy, it does not appear that motion is important to the function of the joint. The older one gets, the more likely that the joint is completely immobile, or ankylosed. Ankylosis is a term that means a joint has become completely stiffened with no movement at all.
Related Document: A Patient's Guide to Lumbar Spine Anatomy
Rationale
What does my physician hope to achieve?
Your doctor is recommending a SI joint injection to try and determine if one, or both, SI joints are the cause of your back pain. This type of injection is primarily a diagnostic injection. The injection may only help your pain temporarily, sometimes just for a few hours. Once your doctor is sure that it is the SI joint causing your pain, other procedures may be recommended to reduce your pain for a longer period of time.
During a SI joint injection, the medications that are normally injected include a local anesthetic and cortisone. The anesthetic medication, such as lidocaine or bupivicaine, is the same medication used to numb an area when you are having dental work or having a laceration sutured. The medication causes temporary numbness lasting one hour to six hours, depending on which type of anesthetic is used.
Cortisone is an extremely powerful anti-inflammatory medication. When this medication is injected into a painful, inflamed joint, it can reduce the inflammation and swelling. Reducing the inflammation reduces pain. If cortisone is also injected into the joint, you may get several weeks' worth of relief from your pain. This can allow you to get started in a physical therapy program, strengthen the muscles, and begin normal movement again. When the cortisone wears off, the pain may not return.
Related Document: A Patient's Guide to Sacroilican Joint Dysfunction
Preparations
How will I prepare for the procedure?
To prepare for the procedure your doctor may tell you to remain "NPO" for a certain amount of time before the procedure. This means that you should not eat or drink anything for the specified amount of time before your procedure. This means no water, no coffee, no tea - not anything. You may receive special instructions to take your usual medications with a small amount of water. Check with your doctor if you are unsure what to do.
You may be instructed to discontinue certain medications that affect the clotting of your blood several days before the injection. This reduces the risk of excessive bleeding during and after the injection. These medications may include the common Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) such as aspirin, ibuprofen, naproxen and many other medications that are commonly used to treat arthritis. If you are taking any type of blood thinning medication you should let your doctor know. You will most likely need to have this medication regulated or temporarily discontinued prior to the injection. Your doctor will need to determine if it is safe to discontinue these medications in order to have the injection.
You may need to arrange to have transportation both to and from the location where you will undergo the injection. Wear loose fitting clothing that is easy to take off and put on. You may wish to take a shower the morning of the procedure, using a bactericidal soap to reduce chances of infection. Do not wear jewelry or any type of scented oils or lotions.
Procedure
What happens during the procedure?
When you are ready to have the injection, you will be taken into the procedure area and an IV will be started. The IV allows the nurse or doctor to give you any medications that may be needed during the procedure. The IV is for your safety because it allows a very rapid response if you have a problem during the procedure, such as an allergic reaction to any of the medications injected. If you are in pain or anxious, you may also be given medications through the IV for sedation during the procedure.
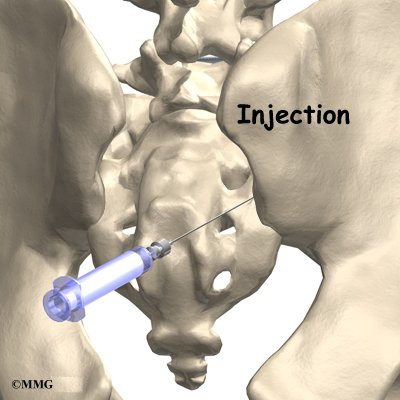
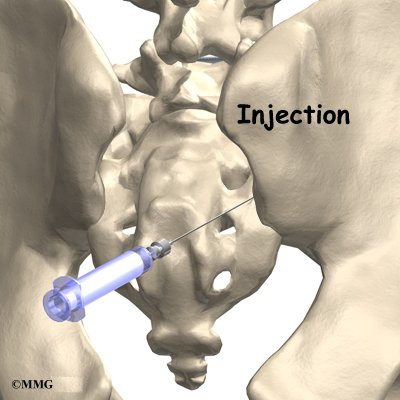
SI joint injections are done with the help of fluoroscopic guidance. The fluoroscope is an x-ray machine that allows the doctor to actually see an x-ray image while doing the procedure. This allows the doctor to watch where the needle goes as it is inserted. This makes the injection much safer and much more accurate. Once the needle is in the right location, a small amount of radiographic dye is injected. Once the needle is in the right location, a small amount of radiographic dye is injected. This liquid dye shows up on the x-ray image and the doctor can watch where it goes. The medication used for the injection will go in the same place, so the doctor wants to make sure that the medication will go to the right place to do the most good. Once the correct position is confirmed, the medication is injected and the needle is removed.
You will then be taken out of the procedure room to the recovery area. You will remain in the recovery area until the nurse is sure that you are stable and do not have any allergic reaction to the medications. The anesthetic may cause some temporary numbness and weakness. You will be free to go when these symptoms have resolved.
Complications
What might go wrong?
There are several complications that may occur during or after the SI joint injection. Injection procedures are safe and unlikely to result in a complication, but no procedure is 100% foolproof. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Complications are uncommon, but you should know what to watch for if they occur.
Allergic Reaction
Like most procedures where medications are injected, there is always a risk of allergic reaction. The medications that are commonly injected include lidocaine, bupivicaine, radiographic dye, and cortisone. Allergic reactions can be as simple as developing hives or a rash. They can also be life threatening and restrict breathing. Most allergic reactions will happen immediately while you are in the procedure room so that help is available immediately. Most reactions are treated and cause no permanent harm. You should alert your doctor if you have known allergies to any of these medications.
Infection
Several types of infections are possible complications of SI joint injections. Any time a needle is inserted through the skin, there is a possibility of infection. Before any injection is done, the skin is cleansed with a disinfectant and the health care provider doing the injection uses what is called a sterile technique. This means that the needle and the area where the needle is inserted remains untouched by anything that is not sterile. The provider may also use sterile gloves.
Infections can occur just underneath the skin, in a muscle, or in the sacroiliac joint. You should watch for signs of increasing redness, swelling, pain, and fever. Almost all infections will need to be treated with antibiotics. If an abscess forms, then a surgical procedure may be necessary to drain the pus in the abscess. Antibiotics will also be necessary to treat the infection.
Increased Pain
Not all injections work as expected. Sometimes, injections cause more pain. This may be due to increased spasm in the muscles around the injection site. The increased pain is usually temporary, lasting a few hours or a few days. Once the medication has a chance to work, the injection may actually perform as expected and reduce your pain. Increased pain that begins several days after the injection may be a sign of infection. You should alert your doctor if this occurs.
After Care
What happens after the procedure?
If everything goes as planned, you will be able to go home soon after the injection, probably within one hour. There are no restrictions on diet or activity after the injection. You can return to physical therapy or chiropractic care as soon as you like.
Your doctor will be interested in how much the pain is reduced while the anesthetic (numbing medication) is working. You may be given a pain diary to record what you feel for the next several hours. This is important for making decisions, so keep track of your pain.
Most doctors will arrange a follow-up appointment, or phone consult, within one or two weeks after the procedure to see how you are doing and what affect the procedure had on your symptoms.
And remember, a sacroiliac joint injection is not a cure for your pain - it is only a part of your overall pain management plan. You will still need to continue working with the other recommendations from your pain management team.
|