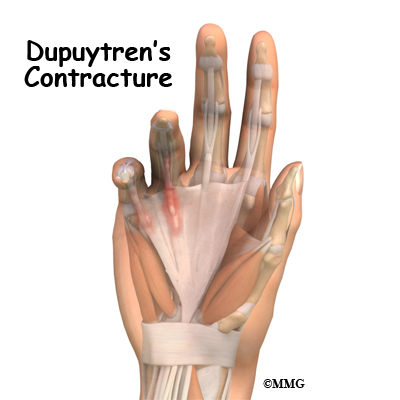
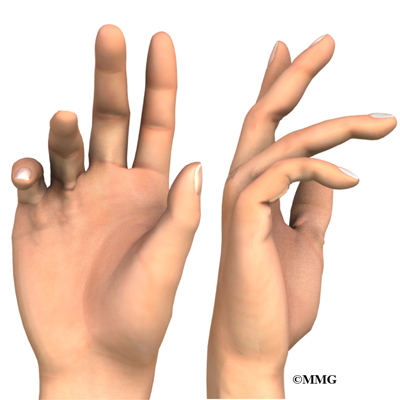
Dupuytren's contracture is a fairly common disorder of the fingers. It most often affects the ring or little finger, sometimes both, and often in both hands. The disorder may occur suddenly but more commonly progresses slowly over a period of years. It is more common in men of a Northern European descent. The disease usually doesn't cause symptoms until after the age of 40.
A partial palmar fasciectomy remains the "gold standard" surgical procedure, although at earlier stages of this disease a less invasive surgical procedure called a needle aponeurectomy may be done.
Surgical treatment does not stop or cure this disease process, so recurrence is not uncommon.
Related Document: A Patient's Guide to Dupuytren's Contracture
This guide will help you understand
- what your surgeon hopes to achieve
- what happens during the operation
- what to expect after the procedure
What is the goal of surgery?
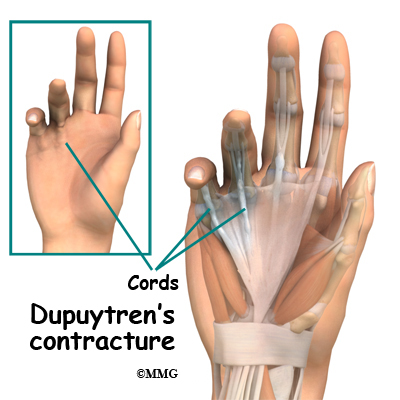
Many cases of Dupuytren's contracture progress to the point where surgery is needed. The goal of surgery is to remove the diseased fascia, allowing the finger to straighten out again. By removing the tight cords and fascia, the tension on the finger is released. Once the fibrous tissue is removed, the skin is sewn together with fine stitches.
In some cases, grafting extra skin is necessary in the area close to the incision to give the finger more flexibility to straighten. Skin grafting is more commonly necessary in severe Dupuytren's contractures that have been present for many years. Over time the skin also contracts. When the contracture or the cord is released, the skin cannot stretch enough to allow the finger to straighten. Skin is added, or grafted into place to allow the finger to straighten without being held back by the skin of the palm.
Preparation
How should I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
Surgery for Dupuytren's Disease is commonly performed as an outpatient - you will probably go home the same day. The surgical procedure may be performed in an operating room in a surgery center or hospital. The needle aponeurotomy may be performed in the office setting. On the day of your surgery, you will arrive at the location chosen by the surgeon and the staff will register and prepare you for the procedure. You shouldn't eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the procedure?
Needle Aponeurotomy (Percutaneous Fasciotomy)
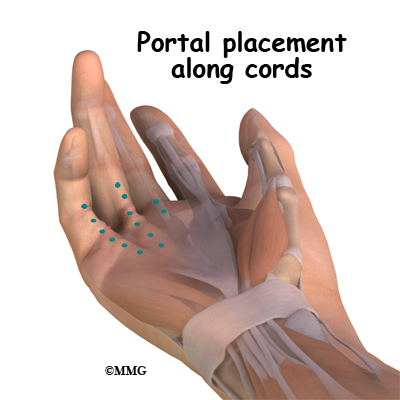
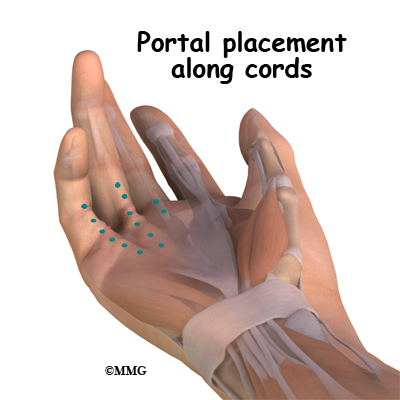
The needle aponeurotomy is available when the disease is at an early stage. Under local anesthesia, the surgeon inserts a very thin needle under the skin. The sharp needle cuts a path through the cord, weakening it enough so that when the surgeon straightens the finger the cord will snap or rupture and allow the finger to straighten. The diseased tissue is not removed. This can be done in an office setting.

Needle aponeurotomy may be used when a patient has a contracture that's due to a palpable cord lying beneath the skin. It does not work for non-Dupuytren's related contractures. The advantage of this procedure is that it can be done on older adults who have other health issues that might make surgery under general anesthesia too risky. The disadvantage is there can be a high recurrence rate because the diseased tissue remains and can continue to contract. There is also the potential for nerve injury, infection, and hematoma (pocket of blood) formation similar to the open procedure.
 Palmar Fascia Removal (palmar fasciectomy)
Palmar Fascia Removal (palmar fasciectomy)
Surgery can last up to 90 minutes. Surgery may be done using a general anesthetic (one that puts you to sleep during surgery), or a local anesthetic (one that only numbs the hand). With a local anesthetic you may be awake during the surgery, but you won't be able to see the surgery.
Once you have anesthesia, your surgeon will make sure the skin of your palm is free of infection by cleaning the skin with a germ-killing solution. An incision will be made in the skin. Several types of incisions can be made, but yours will most likely be made along the natural creases and lines in the hand. This will help make the scar less noticeable once the hand is healed.
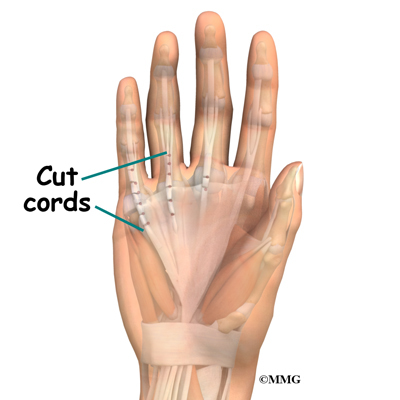
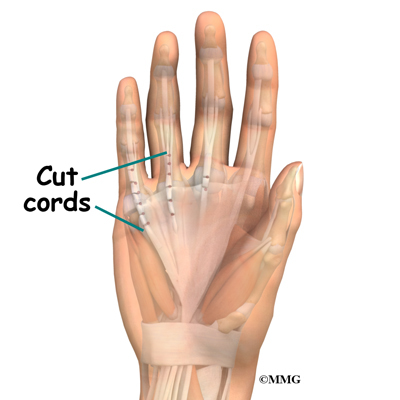
Once the palmar fascia is exposed, it will be carefully separated from nerves, arteries, and tendons. Special care is taken not to damage the nearby nerves and blood vessels.
Then your surgeon will remove enough of the palmar fascia to allow you to straighten your finger. After the diseased tissue is removed, and if the patient has ignored this problem for a long time, the joint capsule or the ligaments of the joint may be stiffened or contracted. Therefore the surgeon may also need to release this tissue in order to allow the finger to straighten up normally. Once the fibrous tissue is removed, the skin is sewn together with fine stitches.
A skin graft may be needed if the skin surface has contracted so much that the finger cannot relax as it should and the palm cannot be stretched out flat. Surgeons graft skin from the wrist, elbow, or groin.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following surgery for Dupuytren's contracture are
- anesthesia
- infection
- nerve and blood vessel damage
Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don't expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Infection of the incision is one possible complication after surgery. Therefore, check your incision every day as instructed by your surgeon. If you think you have a fever, take your temperature. If you have signs of infection or other complications, call your surgeon right away.
Nerve or Blood Vessel Damage
There are many nerves and blood vessels in the hand. It is possible, though uncommon, that these structures can be injured during surgery. If an injury occurs, it can be a serious complication. Injury to nerves can cause numbness or weakness of the hand. Repairing an injury to the blood vessels may require additional surgery.
After Surgery
What happens after surgery?
After a needle aponeurotomy, small adhesive bandages may be applied, or a light gauze wrap. Elevation and ice are recommended for several days following the procedure.
After a partial palmar fasciectomy, your hand will be bandaged with a well-padded dressing and a splint for support after surgery. The splint will keep the hand open and the fingers straight during healing. Your surgeon will want to check your hand within five to seven days. Stitches will be removed after 10 to 14 days, though most of your stitches will be absorbed into your body. Because many nerves are found in the hand, you may have some discomfort after surgery. You will be given pain medicine to control the discomfort.
You should keep your hand elevated above the level of your heart for several days to avoid swelling and throbbing. Keep it propped up on a stack of pillows when sleeping or sitting up.
Rehabilitation
What should I expect during my recovery?
Usually physical therapy is not required after a needle aponeurotomy. NO strenuous gripping for one week. After one week, return to activities as tolerated. Occasionally a splint is prescribed for night use.
After a partial palmar fasciectomy, physical or occupational therapy sessions will be needed for up to six weeks. Therapy visits usually include heat treatments, soft tissue massage, and vigorous stretching. Therapy can make the difference in a successful result after surgery. These sessions are important in limiting the buildup of scar tissue, preventing the return of contractures, and getting the most benefit from surgery.
You'll gradually be able to put your hand to use. You should be able to straighten all joints within four to eight weeks, sometimes a little longer.
You'll probably need to wear a splint at night for up to six months after surgery. It is used to keep the joints straight, preventing new contractures from forming. Take all medicine exactly as prescribed by your surgeon, and be sure to keep all follow-up appointments.